Blog

MRFs
Would Florida Blue Be in the Red if TiC Were Enforced?
This blog post answers a big what-if question: what if the Transparency In Coverage laws were actually enforced and penalties were administered to the entities that are either not posting machine readable files, or are posting files which are obviously incomplete? How financially impacted would those entities be? Read on to see the high level math, as well as our quarterly lay-of-MRF-land with this installment of “MRF Processing Notes”.

Published
4/14/2025
Hi folks, since our last MRF Processing Notes, changes to the TiC data as a whole have been relatively minor. The latest slate of data quality improvements, regressions, and obfuscation tactics are summarized at the end of the post for those of you who care.
Politically, however, quite a bit has changed. The Biden administration has left office and the Trump administration signed a new Executive Order on February 25th announcing that “[US government] departments will update their enforcement policies to ensure hospitals and insurers are in compliance with requirements to make prices transparent” and also noted that “The Trump Administration will work to hold health plans accountable for making drug prices transparent.”
This led our team to thinking - what if the laws were actually enforced and penalties were administered to the entities that are either not posting TiC files, or are posting files which are obviously incomplete? How financially impacted would those entities be? Read on to see the high level math, as well as our quarterly lay-of-MRF-land with this installment of “Processing Notes”.
Macro View of Compliance and Enforcement
In prior blog posts, we’ve covered numerous examples of non-compliance. There are the small plans and rental networks that haven’t posted in ages or have broken hosting pages (Prominence Health Plan, Networks by Design), plans that post broken file or provider reference URLs inside the files (SIHO, LA Care, Amerihealth Caritas), as well as plans that redact provider directory files with asterisks (HMAA, Centivo). These are non-compliant by the obvious definition that you cannot get to a working MRF at all. These are also small plans and networks, on the order of a few tens or hundreds of thousands of covered lives. While they have had years to comply, one might argue they’re also working with small budgets, tech teams, and other constraints, making compliance an outsized relative challenge compared to the BUCAs (shorthand for Blue Cross / United / Cigna / Aetna, our largest health insurers).
Outside of BCBS of Vermont during their Change Healthcare hosting challenges, we’ve tracked no BUCA entities who failed to post any data for a consistent stretch of time. But we do know and have been vocal about some significant Blues who post files each month containing a glaring lack of meaningful data. From the headline you can surmise I’m talking about two prominent examples we have highlighted in the past: Florida Blue and Highmark.
Florida Blue in April 2025 posted a Blue Options PPO file containing just 9,600 NPIs, which is certainly not enough physicians or facilities to treat their almost four million plan members. The file cites 14 available OB/GYNs, 11 available dermatologists, and 16 orthopedic surgeons in the entire PPO network. By comparison, Aetna’s ACA plan in Florida lists 983 orthopedic surgeons, 1796 OBGYNs, and 528 dermatologists - and ACA plans are typically far more restrictive in network access than a commercial PPO.
Highmark of New York posted 24,000 NPIs in their PPO - also a dubious number - but the billing code count in the file is thinner than Florida Blue’s. Highmark cites pricing for just 8300 distinct billing codes, compared to Florida Blue's nearly 18,000, meaning entire swaths of the healthcare procedure set are completely absent from Highmark data.
A cursory web search suggests Highmark revenue last year was ~29.4 billion, and Florida Blue ~32 billion. These entities have the wherewithal to repair their MRF compliance situation, yet both payers have been underreporting in their TiC files since we've been tracking them.
We filed complaints through the official CMS processes, participated in numerous organizations and committees to route concentrated cross-industry feedback to CMS and HHS, and gave numerous talks about issues in the data. We have heard nothing from anyone in an official position about enforcement activity on payer price transparency...until the Trump Executive Order.
Since the Executive Order, there has been renewed activity around prospective enforcement. The agencies charged with enforcement of price transparency regulations have been rapidly circling back to commercial sector players to get feedback on compliance issues. They are asking where schemas are being abused and where rules can be clarified. I surmise these questions are being asked in service of advancing the agenda laid out in the EO. We have been engaged with several CMS leaders alongside many other industry participants, and we are optimistic that the ball is finally rolling on the enforcement side.
Rough Compliance Fine Estimates = Insolvency
So, this brings us to the I-promise-its-not-clickbait headline and thought exercise we started with. What would the financial impact to these entities be if the administration potentially levied the full $100 per member per day noncompliance penalty to these entities on a retrospective basis?
The most recent AIS data suggests Florida Blue has roughly 3.7 million commercial covered lives, while Highmark has roughly 4.2 million. Today is Wednesday, April 9, 2025. TiC started July 1, 2022. That’s 1013 days of running noncompliance. If you multiply those values by $100 per member per day, Florida Blue is eligible for a maximum fine of….drumroll please….$374 BILLION dollars!
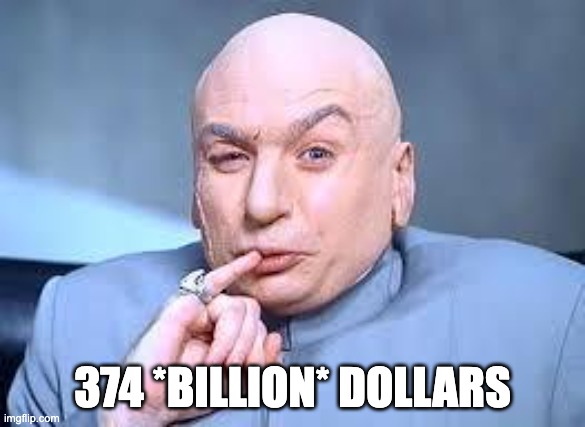

Highmark Health’s potential fine would be even larger at $425 billion. So, to answer the question we started with, YES Florida Blue would be in the red. Deeply in the red. A fine of 10x their entire prior year revenue would put them in a new definitional category of ‘insolvent’...if there is a maximum enforcement action.
What’s More Likely Than Insolvency
Realistically, maximum enforcement is unlikely. If we use the hospital price transparency enforcement actions as a template, there seems to be a process of warning letters and remediation periods before fines are levied, and penalty amounts probably wouldn’t start out at the maximum possible value. But even with significant discounting, any enforcement actions could still result in a fine in the range of tens of millions to low billions of dollars for any noncompliant insurer - certainly not worth ignoring!
There’s also the possibility that health plans recognize the risk and address data quality issues ahead of any enforcement action. Highmark did a call with us back in 2023 and explained some challenges with their FACETS system and on-paper contracts that made compliance difficult, but we haven’t heard much since. Florida Blue responded to us only after the EO was issued.
Still, thekey point is that the EO produced a response. If the teams responsible for generating MRFs at these payers now have the attention and resources (and, probably, plenty of stress and pressure) from their respective organizations to fully comply with the law, it could mean significant improvements in MRF data quality in months to come. And not just from these two plans.
Fixing MRF gaps will be a big undertaking - to anyone on the payer side who might be reading, our team is happy to share metrics on existing files and QA any improvements to your files if helpful.
We are looking forward to seeing how compliance evolves in the coming months, and as usual, we’ll share any statistical changes in future MRF processing notes.
Other Exciting TiC Inventory Updates
On to the meat and potatoes of processing notes blog posts - the who’s and what’s of posting updates, both good and bad.
Good:
- Several smaller BCBS entities greatly improved file contents
- Horizon has reasonable files now for all plans
- Serif Health expanded its library… again!
Bad:
- BCBSTN starts hiding files from their fully insured index
- Blue Shield of California starts masking negotiated rates with ‘100’ values
- Cigna seeing a growth in CSTM-00 percentage arrangements
- Centivo starts masking NPIs a la HMAA
- Healthcare Highways stopped posting its Texas Plus Network
Several smaller BCBS entities greatly improved file contents
This is happy news - we saw quality metric improvements in each of: BCBS of Kansas City, Wyoming, Massachusetts, Minnesota, and Rhode Island. Improvements tended to be less on provider counts and more on codes covered, improving their overall trackable rate counts anywhere by +50% (Massachusetts) to +57,000% relative increases (Minnesota) from previous posting record counts.
Horizon is now producing expected file sizes for all plans
Horizon BCBS of New Jersey tended to post an index with one gigantic indemnity “Trad” INN file (which none of our clients ever want or ask for) and miniscule postings for their other plans which were useless. This past month we saw their other plan IDs suddenly saw file posting sizes on par with the Trad network.
For our commercial customers and clients who have previously been disappointed by Horizon’s data quality, this is a good time to revisit their data and see if new insights are available.
Serif Health expanded its library… again!
We believe one of our key differentiators is a best-in-class data library. We’re always reviewing the latest transparency postings for every plan we can find and adding new plans or shimming non-compliant files to incorporate them in our ever-growing library.
This past quarter, we added new plans from the following payers:
- BlueCross BlueShield of South Carolina
- CenterCare
- Central California Alliance for Health
- Community Health Plan of Washington
- Contra Costa Health
- Evolutions Healthcare Systems
- Group Health Cooperative of Eau Claire
- Healthcare Highways
- Healthchoice
- Horizon Blue Cross Blue Shield of New Jersey
- Independent Health
- Jefferson Health Plans
- Johns Hopkins Health Plans
- Medical Associates Health Plan
- Medical Card System Puerto Rico
- Mountain Health COOP
- MultiPlan
- Preferred Health Professionals
- Samaritan Health Plans
- Viva Health
- Wellpoint
- Zelis
We’re now tracking over 226 payors (with 23 of those flagged as currently non-compliant or non-operating). Exciting stuff!
And now for the bad news.
BCBSTN starts hiding files from their fully insured index
BCBS TN has two different indexes, their ASO index and non-ASO index. The non-ASO index, for several months running, has no TN-speific plan files (their BCBS Entity code is _890_ if you’re looking for it).
It was pointed out by David Muhlenstein of Simple Healthcare that in the ASO index under __HIVE_DEFAULT_PARTITION__index.json (yes, that’s what it's labeled) you can get a full set of in network rates files all helpfully titled “Empty allowed amount file”. Thanks for the tip, David, and here’s hoping this helps other folks trying to find BCBS Tennessee MRFs.
Blue Shield of California starts masking negotiated rates with placeholder value ‘100’
We’re seeing an uptick of reports from many of our customers that BSCA is inserting a placeholder negotiated dollar amount value of ‘100’ in many rates records in their files. Anecdotally, this is even happening for provider and code combinations where accurate rates had previously been reported.
It will be interesting to see if such tough-to-detect masking will have an uptick in a world where enforcement activity is increasing, and lots of entities like ourselves are tracking obvious aggregate metrics like distinct NPI or EIN or code as proxy for data quality. Values like 999999 or 0 are easy to filter out as invalid, but 100 is significantly harder to do since it would be in the valid range for many procedure codes.
Cigna seeing a growth in CSTM-00 percentage arrangements
Some of our customers looking for institutional rates in Cigna have had a difficult time - searching for knee replacement prices in NYC in our API, for example, they only got Veterans Administration hospital rates in return.
The trick is that Cigna posts a substantial portion of their hospital institutional rate records as billing code CSTM-00 with a percentage arrangement. That number has grown, from 4,469 last year to 4,820 records this year. If you’ve been stymied in search of answers for Cigna hospital pricing, that’s the rock to look under. Percentage arrangements are not always useful to data consumers, (i.e. it won’t actually help a Cigna plan member understand what bill they would receive for care in New York City), but at least you know where the hospital rates are.
Centivo starts masking NPIs like HMAA
This one is tough to deal with.Why go through the trouble to produce an MRF file only to go and redact all the NPIs (which are public information, btw) and put yourself back into a fully non-compliant position since no one can use this data? https://eldoradocomputing.hosted-by-files.com/centivopublicACTBL/2025-04-01_Activision-Blizzard_provider-reference.json

HMAA and Centivo are the two plans that clearly do this - but it needs to be fixed if this data can ever be useful to consumers.
Healthcare Highways stopped posting its Texas Sync INN file
Healthcare Highways is a network that we see a lot of requests for on the employer side of the house. They’ve produced a really clean and compliant MRF for years. We can still find the Oklahoma HCH Plus network file just fine, but the Sync network file has gone missing as of last November.
If anyone knows where to get a recent 2025 copy, hit me up and I’ll buy you a coffee!
Takeaways
Well, that’s all for this quarter folks. Hope the thought exercise on fines was illustrative for all those non-compliant plans out there, and spurs any such plans to start producing complete files ASAP. Should enforcement plans get crystallized by the Trump administration over the coming months, the potential penalties could be massive.
I also hope our processing notes are helpful to all our fellow MRF collectors and consumers out there. We’re all in the data maze together.
Prospective clients and customers - if our expertise working with this data can be useful to your organization, if you’ve been unsatisfied with Horizon data in the past, or any of our new plans or networks have been on your wish list, it’s a great time to get in touch with our team!